How Does Genetic Cancer Screening Work?
Recent advances in DNA sequencing and analysis make it faster, easier and more affordable than ever before to screen a single patient for adverse mutations in a whole host of genes associated with an increased risk of developing cancer.

Recent advances in DNA sequencing and analysis make it faster, easier and more affordable than ever before to screen a single patient for adverse mutations in a whole host of genes associated with an increased risk of developing cancer. Importantly, hereditary cancer screening allows patients and their physicians to take a proactive approach in effectively managing cancer syndromes by identifying specific inherited gene mutations and the risks associated with those mutations. So what kind of wizardry is required to perform genetic cancer screening? Let us take you on a short tour of the process as we perform it here at Kailos, beginning with the source material for every hereditary cancer test: patient DNA.

Hereditary cancer syndromes are familial, meaning that a parent with an adverse variant or “misspelling” of a gene is capable of passing that same gene mutation on to their child. In hereditary cancers, these gene misspellings are often in genes associated with controlling cell growth and/or division. When a child inherits an adverse gene mutation from their affected parent, every cell in the child’s body possesses a gene with an impaired ability to control cell growth or division, predisposing that child to cancer. Normal cells accumulate mutations over time, and if enough genes controlling cell growth or division are adversely affected, a normal cell will become cancerous and divide uncontrollably.
Because hereditary cancer syndrome gene mutations are present in every cell in an affected individual from birth, we are able to acquire, sequence and analyze DNA from any somatic (nonreproductive) cell in the body to determine what gene mutations that individual possesses. One of the easiest and fastest ways to obtain patient cells is by collecting cheek (buccal) cells using a sterile cotton swab. Every cheek cell present on the swab contains the patient’s entire genome, or every gene in the patient’s body. Once the buccal swab reaches the lab, the swab sample is processed to release the DNA from the buccal cells and purify it sufficiently for DNA sequencing.
Sequencing DNA
We need to sequence a patient’s DNA, or determine the exact order of As, Cs, Gs and Ts in their genes, to determine which gene mutations that person possesses. Once the lab has sufficiently purified a patient’s DNA, specific genes associated with heritable cancer syndromes are targeted and amplified (copied many times) to provide robust DNA sequencing results. The targeted DNA is then sequenced using Illumina NextGen sequencing technology, where an incredibly large number of short strands of DNA are attached vertically to an array and a specific wavelength of light is detected by highly sensitive optics with the addition of each nucleotide, or A, C, G and T, along the length of each DNA strand, determining the exact sequence of the patient’s DNA. Once the sequencing run is finished, the quality of the sequence data is verified and the many short stretches of DNA sequence are assembled using computer software to construct the patient’s larger target DNA sequence, or those genes or parts of genes associated with hereditary cancer syndromes.
Determining Variants
In order to determine whether or not a patient possesses a hereditary cancer syndrome gene mutation, we need to compare the patient’s DNA sequence to a reference DNA sequence without hereditary cancer syndrome mutations. Analytical software allows us to align patient DNA to reference DNA to identify any variants, or differences, between the two, including single nucleotide mutations (misspellings), deletions (one or more nucleotides missing from a gene) or insertions (one or more nucleotides added to a gene).
Importantly, not all variants identified during patient DNA sequencing and analysis will be associated with an increased risk of developing cancer. Some variants have already been researched by scientists and clinicians and these studies can guide scientists when assessing the risk associated with that particular gene mutation. The NIH curates a database, ClinVar, to provide up-to-date information regarding known genetic variants. When variants have not been previously studied or described, scientists analyze the effect of the variant on the functionality of the gene product, or protein. Gene insertions and deletions, in particular, can have a profound effect on gene functionality by completely changing the sequence of a protein downstream of a gene insertion or deletion or prematurely truncating a protein. Alternatively, a variant may change a single amino acid in a protein and the effect of this change can be much more difficult to predict.
Reporting the Results
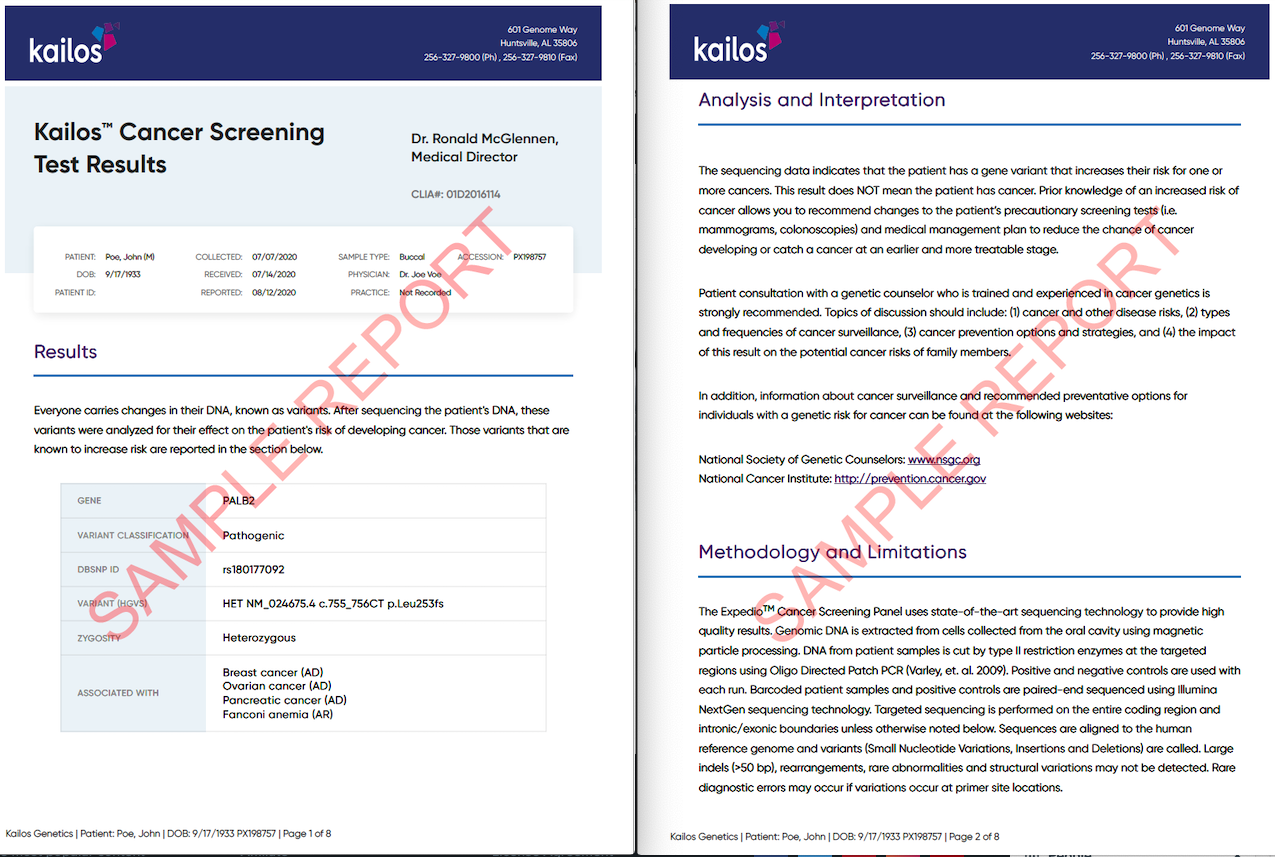
Currently, the only genetic cancer screening variants that are reported by Kailos scientists are those with sufficient evidence in the ClinVar database to be deemed pathogenic or likely pathogenic, or mutations that either truncate or significantly change the protein sequence and likely render the gene product nonfunctional. Those variants that are considered harmless (benign) or likely benign are not reported, and variants of unknown significance (VUS), meaning it is unknown whether or not the mutation is harmful, are also omitted from reporting. Each hereditary cancer screening report details the characteristics of each pathogenic or likely pathogenic variant found after the sequencing and analysis of the patient’s DNA and the hereditary cancer syndrome associated with that particular variant.
Reading the Report
We recommend that patients go over their report with their physician or other designated medical professional, such as a genetic counselor, in order to fully understand the implications of their hereditary cancer test results. Genetic cancer screening reports outline:
1) the specific gene mutations, if any, present in the patient’s genome,
2) the hereditary cancer syndromes associated with the gene mutations and
3) the increased risk of developing specific cancers with each hereditary cancer syndrome.
Additionally, the report describes disease management options to mitigate risk and the inheritance pattern of the mutation to help determine how the mutation could affect other members of the patient’s family. We also include a complete list of all of the genes sequenced and analyzed for the screening and a brief description of our DNA sequencing and analysis methods. Portions of a sample report can be viewed below. Critically, genetic testing results indicating an individual possesses a variant associated with an increased risk of developing cancer does not mean the individual has cancer; rather, the test indicates that the individual possessing the variant is more likely to develop certain cancers during their lifetime.
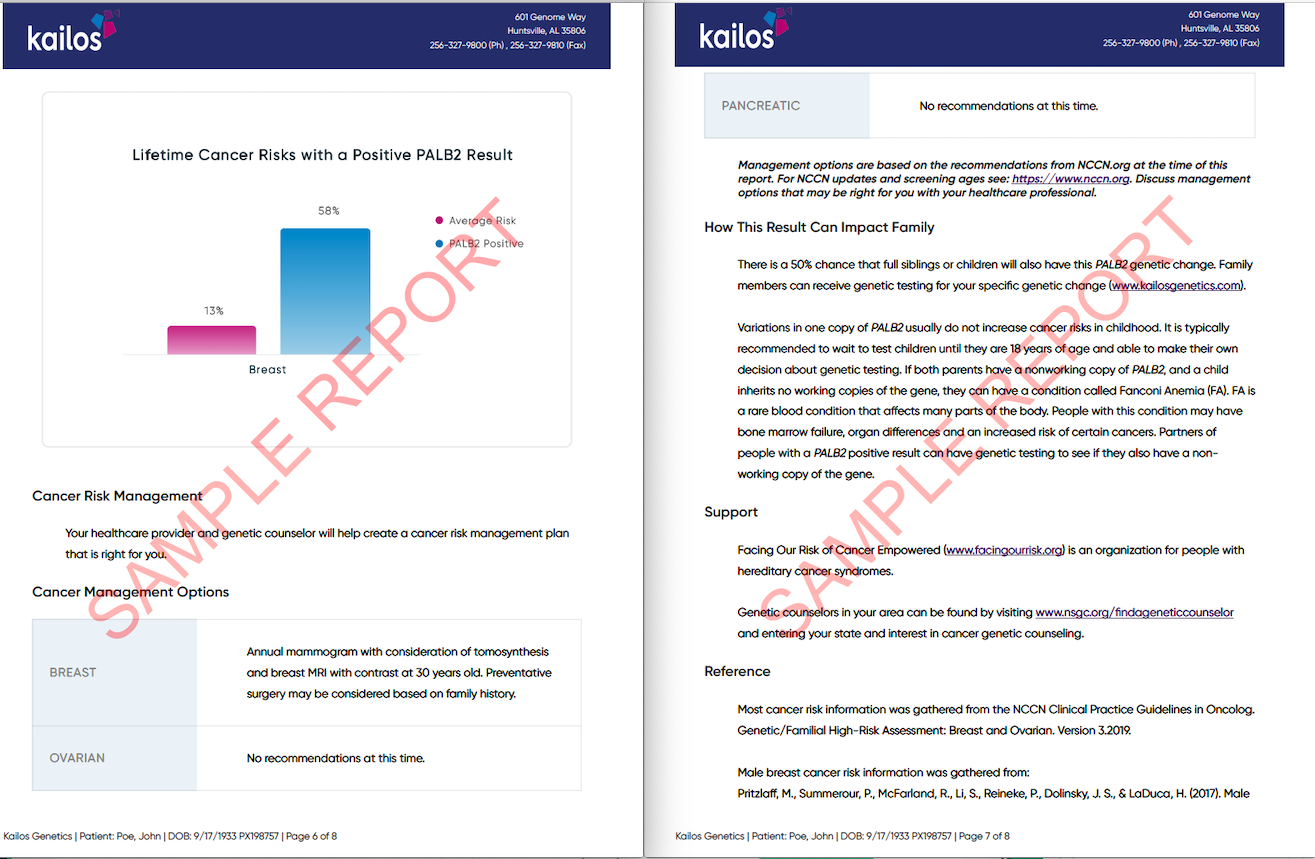
The power of hereditary cancer screening is severely limited without a carefully formulated disease management and prevention plan, which is only possible when patients use their genetic testing information and work to proactively manage disease with their physician. Patients and their physicians can outline healthcare strategies based on the patient’s increased cancer risk, treatment tolerance and goals. In some cases, management of cancer syndromes may depend solely on earlier disease surveillance, in order to detect cancer at an earlier and more treatable stage, whereas preventative procedures and therapies may be available for other hereditary cancer syndromes. Kailos Genetics’ hereditary cancer screening, ExpedioTM, is designed to give every patient the information they need to proactively manage an inherited predisposition for cancer together with their physician. Click here to learn more about ExpedioTM or contact us with any questions you have regarding our company or our genetic tests.